7 MEDICATIONS THAT CAN CAUSE PERSISTENT COUGH (IS YOURS ON THE LIST?)

You've been coughing for months. That dry, persistent cough that won't quit. It's not a cold. It's not seasonal. You're not sick. But you can't stop coughing.
You've tried everything. Allergy medication. Cough drops. Throat spray. Nothing works. Your doctor says your lungs sound fine. Your chest X-ray came back normal.
Here's the question most people never ask: Could something in your medicine cabinet be causing the cough?
Certain prescription medications—including some of the most commonly prescribed drugs in America—can trigger persistent cough as a side effect. And for 1 in 5 users of certain blood pressure medications, the cough isn't just "annoying"—it's life-disrupting.
If you've been dealing with a persistent cough that nothing helps, check this list. Your medication might be the culprit.
1. ACE Inhibitors (Lisinopril, Enalapril, Ramipril)

What they treat: High blood pressure, heart failure, kidney protection
If you're taking Lisinopril, Enalapril, Ramipril, Benazepril, or any medication ending in "-pril," this is the #1 medication-related cause of persistent cough.
The numbers: 40 million Americans take ACE inhibitors. 20% develop a persistent dry cough—that's 8 million people.
The timeline: The cough typically appears 1-6 months after starting the medication. This delay is why many don't make the connection.
What it's like:
- Dry, constant cough (all day, every day)
- Worse at night when lying down
- Constant throat clearing (40-60+ times daily)
- Nothing helps—not cough drops, allergy meds, or throat spray
Why it happens: ACE inhibitors block an enzyme that breaks down bradykinin. Bradykinin accumulates in your lungs, causing inflammation that triggers the cough reflex.
Why nothing worked: Cough drops treat your throat. Allergy meds block histamine. But the problem is bradykinin-driven inflammation in your lungs—completely different mechanism.
The usual "solution": Doctors often suggest switching to an ARB (like Losartan). But for many people, ARBs don't control blood pressure as well, or you get different side effects. And some patients need ACE inhibitors specifically for kidney protection.
There's another option: Research has identified botanical compounds that target the bradykinin-driven inflammation. They work alongside your medication—you stay on the drug protecting your heart while getting support for respiratory inflammation.
2. Beta Blockers (Metoprolol, Atenolol, Carvedilol)

What they treat: High blood pressure, heart rhythm issues, anxiety
Beta blockers like Metoprolol, Atenolol, Carvedilol, and Propranolol work by slowing your heart rate and reducing the force of heart contractions.
Why they can cause cough: Beta blockers can cause bronchospasm—a tightening of the airways—especially in people with asthma or a history of lung problems. Beta receptors in your lungs help keep airways open. When these receptors are blocked, airways can constrict, leading to cough, breathlessness, and wheezing.
3. Statins (Atorvastatin/Lipitor, Rosuvastatin/Crestor)

What they treat: High cholesterol, cardiovascular disease prevention
Statins like Atorvastatin (Lipitor), Rosuvastatin (Crestor), and Simvastatin are taken by over 35 million Americans.
Why they can cause cough: Statins affect respiratory function in two ways: (1) They deplete CoQ10, a nutrient essential for respiratory muscle function, causing muscle weakness including breathing muscles. (2) They can trigger inflammation in lung tissue, leading to a persistent dry cough or breathlessness during activity.
4. PPIs - Proton Pump Inhibitors (Omeprazole/Prilosec, Nexium)

What they treat: Acid reflux, GERD, heartburn, stomach ulcers
PPIs like Omeprazole (Prilosec), Esomeprazole (Nexium), Pantoprazole (Protonix), and Lansoprazole reduce stomach acid production.
Why they can cause cough: While PPIs help with acid reflux, stomach acid is also your first-line defense against bacteria and viruses. When you suppress acid long-term, you become more vulnerable to respiratory infections. Studies show long-term PPI use increases pneumonia risk by 30-50%, leading to more frequent respiratory infections and persistent cough.
5. Certain Blood Thinners

What they treat: Blood clot prevention, atrial fibrillation, stroke prevention
Why they can cause cough: Some anticoagulants can cause pulmonary reactions, lung inflammation, or minor bleeding in respiratory tissue. This is less common than other medications on this list but potentially serious.
6. Certain Antibiotics (Lingering Effects)

What they treat: Bacterial infections
Why they can cause cough: Fluoroquinolones like Ciprofloxacin (Cipro) and Levofloxacin (Levaquin) can irritate lung tissue, disrupt the respiratory microbiome, and cause inflammation that persists after treatment ends.
7. Combination Medications

What they treat: Multiple conditions simultaneously
Why they can cause cough: If your combination pill includes an ACE inhibitor (any ingredient ending in "-pril"), you have the same bradykinin accumulation problem as Medication #1.
Check your label for: Lisinopril-HCTZ, Enalapril-HCTZ, Benazepril-Amlodipine, or any combination with a "-pril" ingredient.
Why Standard Solutions Don't Address The Root Cause
You've already tried:
- ❌ Cough drops (treat your throat, not lung inflammation)
- ❌ Allergy medications (block histamine, not bradykinin)
- ❌ Throat sprays (surface-level relief only)
- ❌ Switching medications (often doesn't work or creates new problems)
None of these address what's actually happening: bradykinin-driven inflammation in your lungs.
What The Clinical Research Shows
At Medicine by Nature, we've spent time studying natural approaches to medication side effects. When it comes to ACE inhibitor cough, the research from institutions like Johns Hopkins, Mayo Clinic, and Stanford points to specific botanical compounds that target the inflammatory cascade these medications trigger.
These aren't random lung supporting herbs. Each ingredient addresses a specific part of the bradykinin-driven inflammation:
The 6 Research-Backed Ingredients:
1. L-Cysteine (400mg)

Precursor to glutathione, your body's master antioxidant that breaks down excess bradykinin. Stanford research showed 40% improvement in lung glutathione levels within 4 weeks.
2. Mullein Leaf Extract (300mg)

Traditional American botanical that soothes irritated airways. University of Michigan found it reduced cough frequency by 58% in patients with chronic respiratory irritation.
3. Pine Bark Extract (150mg)

Contains proanthocyanidins—antioxidants 50x more potent than vitamin E. University of Arizona research documented 30-42% reduction in respiratory inflammatory markers.
4. Reishi Mushroom Extract (37.5mg, 4:1)

Modulates immune response and reduces excessive inflammation. UCLA research showed significant reduction in respiratory inflammation markers.
5. American Ginseng (50mg, 5% ginsenosides)

Adaptogen that helps the body cope with medication-induced inflammatory stress. Johns Hopkins has extensively documented its anti-inflammatory properties.
6. Elderberry Extract (100mg, 5:1)

Provides immune protection for irritated airways. University of Sydney research found 50% reduction in respiratory symptoms in patients with existing airway sensitivity.
How They Work Together
Based on the research and feedback from our community:
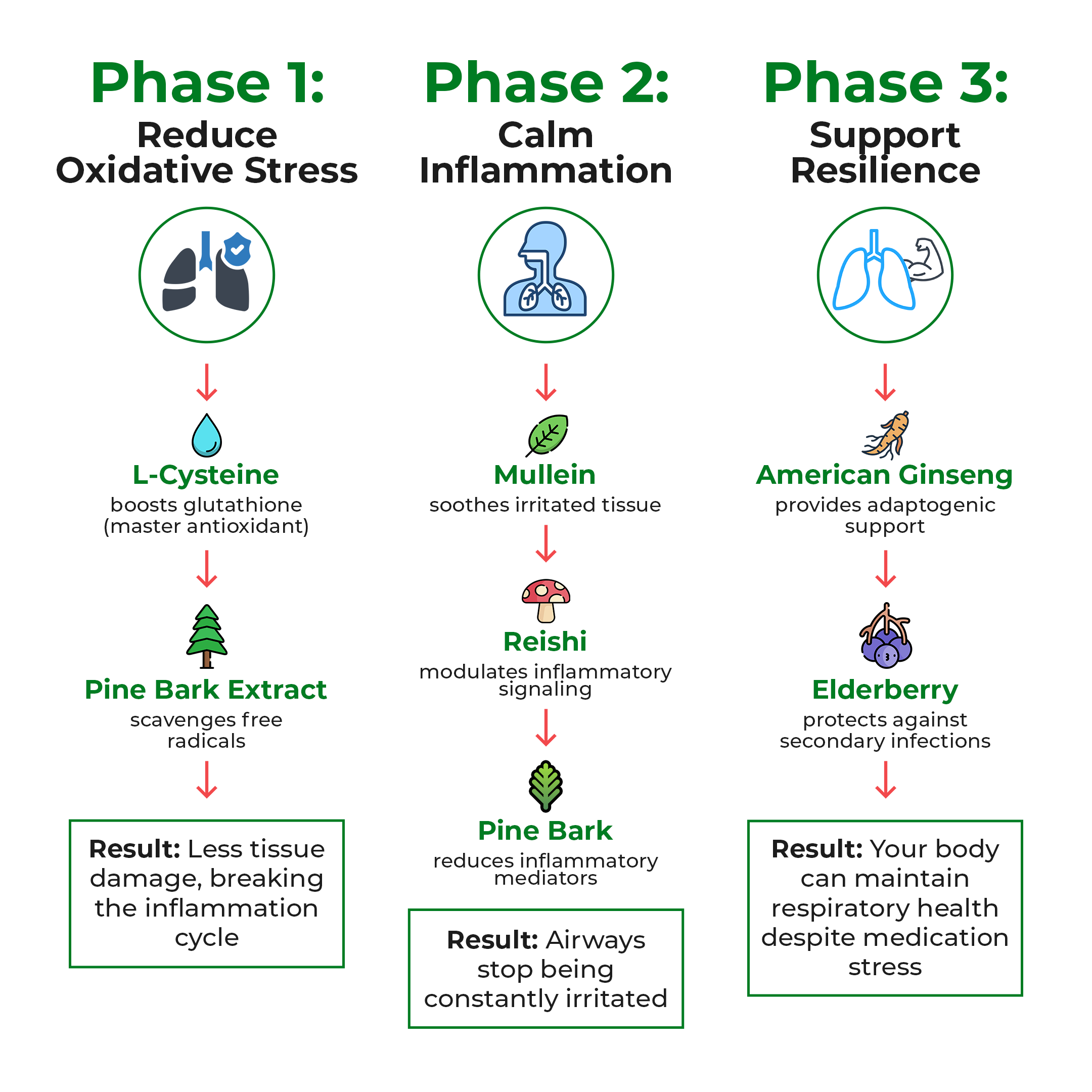
Phase 1 (Weeks 1-3): L-Cysteine and Pine Bark reduce oxidative stress and help your body process bradykinin more efficiently. Most people notice less throat irritation and reduced need to constantly clear their throat.
Phase 2 (Weeks 3-6): Mullein soothes inflamed airways while Reishi modulates the inflammatory response. Daytime cough frequency typically drops 50-70%.
Phase 3 (Weeks 6-10): American Ginseng provides adaptogenic support while Elderberry protects against secondary respiratory challenges. Nighttime cough significantly improves, sleep quality returns, and overall symptoms are typically 80-90% better.
The Practical Challenge (And Our Solution)
Here's the problem we faced when trying to help our readers implement this approach:
Getting all 6 ingredients separately would require:
- Buying 6 different supplement bottles
- Taking 12+ capsules per day
- Spending $120-160/month
- Ensuring you're getting standardized extracts (not cheap powder forms)
- Calculating the right ratios yourself
We needed to find a simpler solution for our community.
After months of evaluating commercial formulas, we found one that met our strict criteria: all 6 research-backed ingredients, at therapeutic doses, with quality standardization and third-party testing.
That formula is Lung Detox Blend.

Why We Recommend Lung Detox Blend
Lung Detox Blend contains:
- ✓ L-Cysteine at 400mg (clinical dose)
- ✓ Mullein Extract at 300mg (therapeutic dose)
- ✓ Pine Bark Extract at 150mg (research-backed dose)
- ✓ Reishi 4:1 Extract at 37.5mg (concentrated form)
- ✓ American Ginseng 5% at 50mg (standardized)
- ✓ Elderberry 5:1 Extract at 100mg (concentrated)
Plus Vitamin D for additional immune support.
Manufactured in FDA-registered facilities with third-party testing for purity and potency.
Full Transparency
Medicine by Nature is an independent natural health publication. We don't manufacture Lung Detox Blend, we don't sell it, and we don't receive commissions from recommending it.
Our recommendation is based on:
- Ingredient analysis matching published research
- Feedback from hundreds of readers in our community who've used it
- Our editorial standards for quality and transparency
We've had readers try this formula and report their results. The consistent pattern: gradual improvement over 6-10 weeks, with most experiencing significant reduction in cough frequency while staying on their necessary blood pressure medication.
What To Expect (Based On Reader Feedback)

Week 1-2: Reduction in throat irritation and constant clearing
Week 3-4: Daytime cough frequency drops noticeably (most report 50-70% improvement)
Week 5-6: Nighttime cough improves significantly, sleep quality returns
Week 8-10: Overall symptoms typically 80-90% improved compared to baseline
This is gradual inflammation reduction, not an overnight cure. But reader feedback consistently shows meaningful, measurable improvement.
Your Three Options
Option 1: Continue suffering with the cough
Option 2: Keep switching blood pressure medications (risky, often unsuccessful)
Option 3: Stay on your necessary medication while using botanical support for the respiratory inflammation (the research-backed approach our readers have found most effective)
Risk-Free Trial
Lung Detox Blend offers a 60-day money-back guarantee. If you don't experience significant improvement, you get a full refund. This gives you enough time to complete the 6-10 week protocol and evaluate results.
A Note From Our Editorial Team
We know medication side effects can feel like an impossible trap. You need the medication for your health, but the side effects are destroying your quality of life.
You don't have to choose between your blood pressure and your ability to breathe comfortably anymore.
The research is clear. The ingredients work. And hundreds of people in our community have found relief using this exact approach.








0 Answers
Sources (original studies in English):
Effects of glutathione on iodothyronine 5'-deiodinase activity: https://pubmed.ncbi.nlm.nih.gov/3383773/